Breaking Down Discharge Function Score (DFS) for Home Health
With the new Discharge Function Score measure now included in SHP reports, many have asked “What do we do at the agency level?”
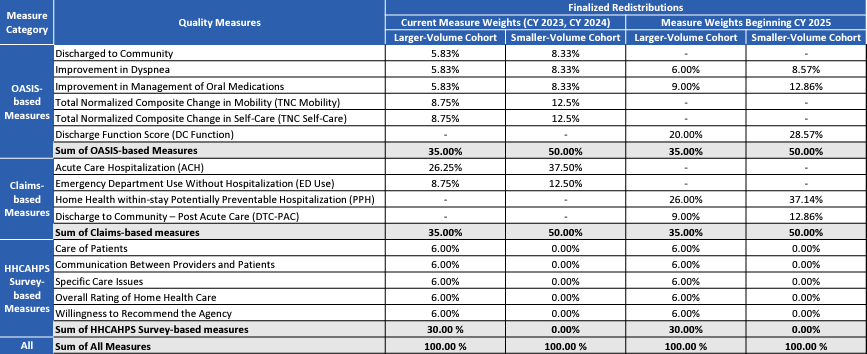
One of the most impactful things you can do is to educate your staff about the new measure. In order to understand why DFS is important, let them know it’s a part of Home Health Value Based Purchasing (HHVBP). A simplified way of educating your staff about HHVBP is to explain that reimbursement is tied to the quality of care we provide to our patients. DFS accounts for a significant amount weighing in at 20%.
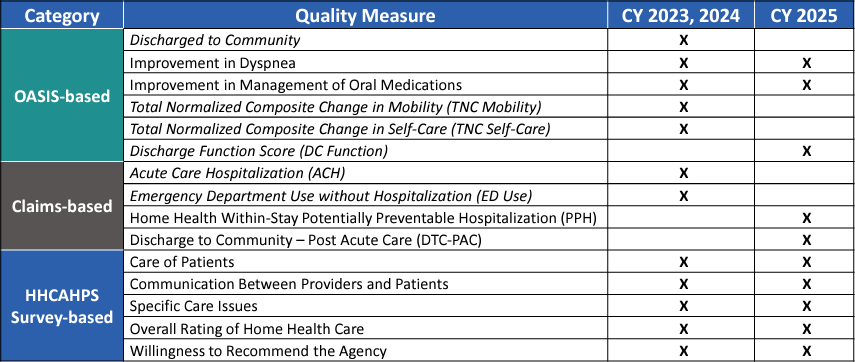
Measure Weights
DFS is determined by assessing 10 measures (Eating, Oral Hygiene, Toileting Hygiene, Roll Left and Right, Lying to Sitting on Side, Sit to Stand, Chair/Bed-to-Chair Transfer, Toilet Transfer, Walk 10 Feet, Walk 50 Feet with 2 Turns, and Wheel 50 Feet with 2 Turns for Non-ambulatory Patients). Clinicians enter scores at SOC, which are processed through a complex CMS’ algorithm to produce an Expected Score of performance by discharge. Inform staff that CMS will remove the DC Goal they are accustomed to answering, and that the measure is met if you meet or exceed that Expected Score.
In review of the 10 measures, there are similarities that can make achieving expected scores easier. When discussing with staff, make it positive and point out the similarities. For example, if you look at the individual GG measures, Eating and Oral Hygiene have similar muscle movement. So, if they improve on one measure, they likely will improve both! Another example would be that clinicians are accustomed to working on improving the Transferring M item. If they can improve Transfers, they are essentially improving 5 of the GG items in DFS (this includes Toilet Transferring as it is essentially the same as Bed/Chair Transferring). Since many items are so closely related, it’s easier to meet expected scores! This is a great opportunity to get OT’s involved as their focus is on upper body training!
Remember to let field staff know that the Expected Score is not calculated in SHP reporting until the associated SOC/ROC assessment information is received, so they may not see the score immediately. This is where weekly case conferences will help. It’s also a great opportunity to inform staff what Expected Scores are, so they can work towards meeting them and to answer the question “Do we have the correct staff caring for the patient to reach the expected score?” You may also find it helpful to create another form of communication, such as an admission chat, document the expected score in the EMR, etc. – any creative way to help keep staff informed. As discussed in a recent SHP’s DFS webinar (login required), please bear in mind the importance of communicating to all staff. The OASIS clinicians are scoring, but LPN’s, PTA’s, COTA’s, Aides and Social Workers play an integral part in success as well.
CMS risk-adjusts certain factors like age, prior surgery, cognitive function among many others in the algorithm used to produce the Expected Score. CMS is now providing us with where they expect the patient to functionally be at by discharge, which is a new approach for home health. Also keep in mind, you could improve a patient in some of the items, but not in all of them, and still meet the CMS Expected Score, and thus meet the DFS measure. The key is assessing correctly on SOC/ROC.
Teach staff to avoid the Activity Not Attempted (ANA) response as much as possible when assessing their patients and documenting the GG items. Let them know that CMS will provide a score that is derived by an estimation through statistical imputation. This could potentially lead to a higher expected score they cannot reach. If they understand that CMS is assigning a score, they may be less apt to use them.
To optimize workflows, conduct comprehensive reviews of GG items at SOC, ROC, and DC. Utilize SHPS’s Episode Einstein tool for a quick view and to compare GG and M items for potential discrepancies. Analyze the Outcome Patient Detail Reports to identify trends and areas for improvement as we break the measure down into each of the GG item components.
As always, it is important to remind your staff that they take excellent care of their patients, and typically achieve improvement – we just need to be sure that this is accurately reflected in documentation as well.
With the DFS measure available in SHP reporting today, we are here to help support you in getting a head start on key workflows to help ensure consistently higher scores. We encourage you to use the next several months to review DFS scores, educate staff, and determine your best plan of action and monitoring to be successful in the upcoming year.
Comparison of Applicable Measure Sets: CY 2023, CY 2024, and CY 2025