CMS Proposes to Overhaul HHVBP
In the CY 2018 Home Health Proposed Rule, CMS is dramatically changing the scoring methodology for the pilot program known as the Home Health Value-based Purchasing Program (HHVBP). This is a Center for Medicare and Medicaid Innovations (CMMI) program designed to test paying for “value” at higher levels of bonuses and penalties, compared to other health sector VBP programs, to see if it incentivizes provider behavior. What is striking to me is that these changes are being made during the fourth year of the five-year program, where up to 7% of Medicare revenues are at risk.
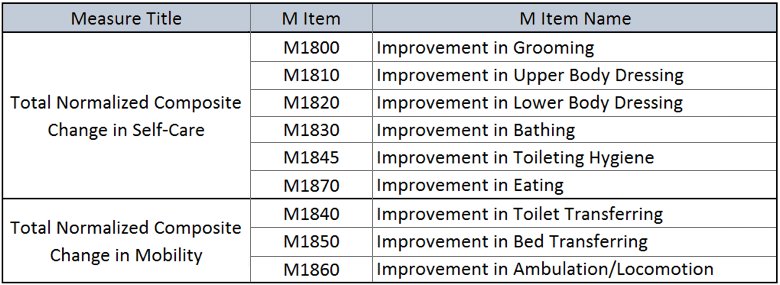
Last year, CMS proposed and implemented one change to the HHVBP program. As of performance year three (CY 2018), CMS eliminated the Drug Education on All Medications Provider to Patient/Caregiver measure as one of the 17 OASIS/HHCAHPS and claims-based measures. This was a relatively low-impact change since the measure was topped out and had little effect on the overall scoring. This year however, the changes are much more dramatic. CMS is proposing to eliminate 5 measures and add two new composite ones made up of six and three measures respectively (see table).
The calculations used for the composite measures are very complicated and both will be risk-adjusted. In the proposed rule, CMS did not share examples of what these scores would look like nor any national provider distributions using prior year(s) data. I can imagine providers in the nine HHVBP states have no idea how these composite scores may impact their overall TPS scores. This is no doubt a very concerning situation for many providers given that 7% of their Medicare revenue is at risk.
In addition, whereas today the existing 16 OASIS/HHCAHPS and claims measures all have equal weights in rolling up their scores into a Total Performance Score (TPS), the weights are proposed to be adjusted to emphasize the claims-based measures. The proposal is to weight the two claims-based measures at 35%, the five HHCAHPS measures at 30% and the six OASIS measures at 35%. The 60-day hospitalizations will also be re-weighted to contribute 75% of the overall 35% weight given to the two claims-based measures, increasing the weight from 6.25% to 26.25%. The impact can even be greater depending on if the agency is exempt from participating in the HHCAHPS due to low patient census. Without HHCAHPS scoring, the weighting of the 60-day hospitalization measure increases to 37.5%.
Finally, CMS is proposing to cap the number of points a provider can earn on improving their scores over their base year from 10 to 9 points. CMS noted it would encourage providers to focus more on achieving higher performance levels (to get the 10 points) and less on their improvement.
With so much at stake, the National Association for Home and Hospice Care (NAHC) commented on the proposed rule regarding their “concerns with incorporating into the HHVBP model a composite self-care measure that uses outcome measures that are not currently included in the HHVBP model and have not been a priority focus for quality improvement for agencies participating in the HHVBP program.” NAHC is also recommending a delay by one year in implementing the change to the weighting methodologies.
With the final rule due out around the end of October, we will have to wait and see if agencies will have the time to adjust to the impact of these proposed HHVBP changes.

