Hospice Proposed Rule has QRP Updates with no HEART
On April 28th, CMS issued the FY 2019 Hospice Payment and Quality Reporting proposed rule. Along with the typical annual payment updates, there were new proposals to the Hospice Quality Reporting Program (HQRP) for consideration, but no mention of the Hospice Evaluation and Reporting Tool (HEART). The HEART was first proposed last year in promoting a new assessment tool that would allow for more quality measures in Hospice.
As expected, CMS announced that the HQRP public reporting will include the new Comprehensive Assessment Composite Measure and Visits When Death is Imminent Measure Pair on Hospice Compare in the fall of 2019. At the same time, CMS will remove the detail of the 7 Hospice Item Set (HIS) measures that make up the Composite, although a link to an expanded view of the detail will be available.
CMS provided some data as to how hospices are performing on the three new measures. Based on our SHP national database, we looked to see what the real time improvements were in these new HQRP measures over the last four quarters (see graph).
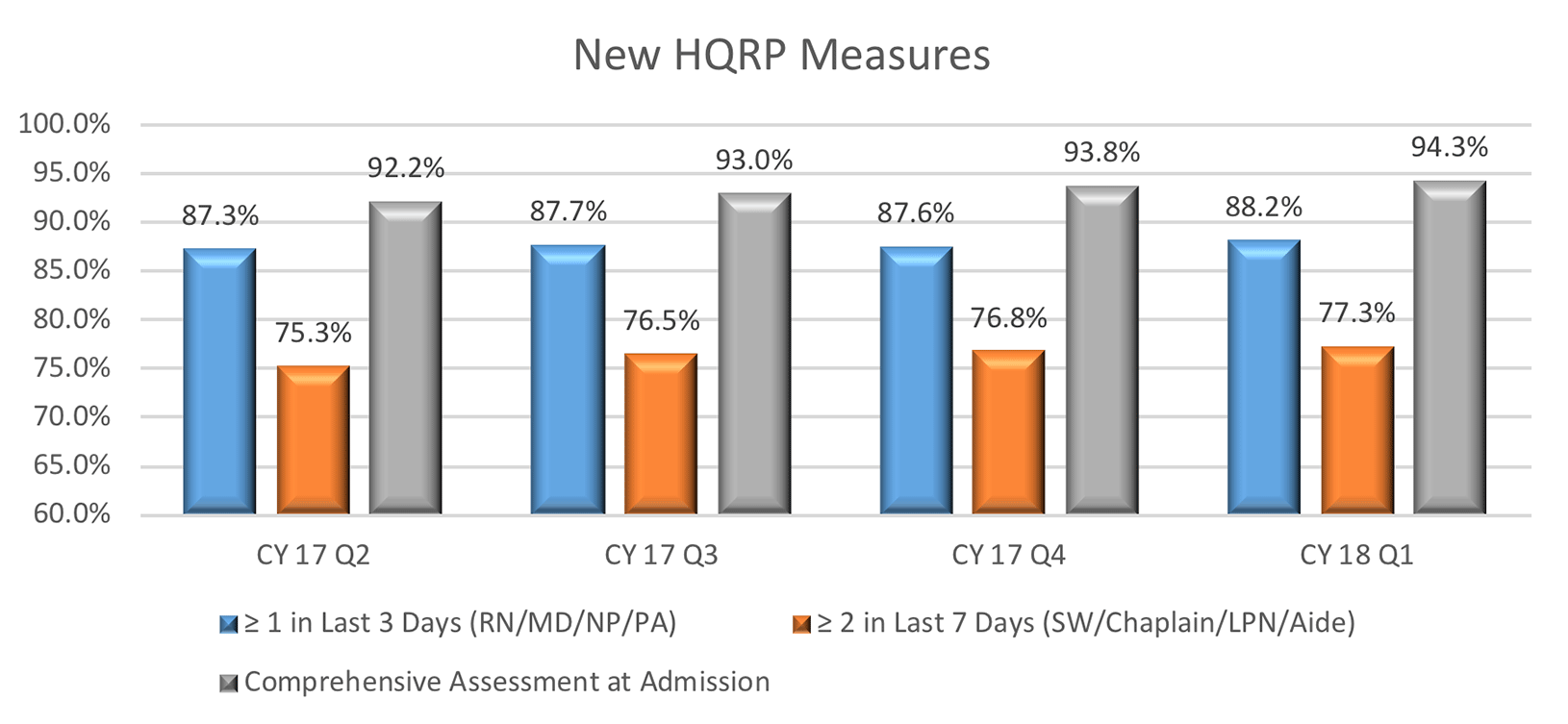
Across all three measures, hospices have shown improvements in each of the last four quarters: 0.9% in Visits in the last 3 days; 2.0% in Visits in last 7 days; and 2.1% in the Comprehensive Assessment.
CMS proposed other updates to the hospice reporting of the HIS for patients. Whereas currently hospices have up to 3 years to update and correct HIS records, CMS is proposing that hospices will now need to correct and report all changes within 4-½ months from the end of any quarter in order for the change to be reflected on Hospice Compare. This will take effect starting in January 1st, 2019 for quarter ending March 30th, 2019. For this first quarter, all corrections will need to be made by August 15th, 2019. This change aligns with other post-acute care programs that already have this requirement.
CMS also provided some insights into how they plan to improve patient outcomes and reduce provider burden through “meaningful measures”. CMS noted that the “Meaningful Measures Initiative represents a new approach to quality measures that fosters operational efficiencies, and will reduce the costs including collections and reporting burden, while producing quality measurement that is more focused on meaningful outcomes.”
| Quality Priority | Meaningful Measure Area |
|---|---|
| Making Care Safer by Reducing Harm Caused in the Delivery of Care | Healthcare-Associated Infections |
| Preventable Healthcare Harm | |
| Strengthen Person and Family Engagement as Partners in Their Care | Care is Personalized and Aligned with Patient’s Goals |
| End of Life Care according to Preferences | |
| Patient’s Experience of Care | |
| Patient Reported Functional Outcomes | |
| Promote Effective Communication and Coordination of Care | Medication Management |
| Admissions and Readmissions to Hospitals | |
| Transfer of Health Information and Interoperability | |
| Promote Effective Prevention and Treatment of Chronic Disease | Preventive Care |
| Management of Chronic Conditions | |
| Prevention, Treatment, and Management of Mental Health | |
| Prevention and Treatment of Opioid and Substance Use Disorders | |
| Risk Adjusted Mortality | |
| Work with Communities to Promote Best Practices of Healthy Living | Equity of Care |
| Community Engagement | |
| Make Care Affordable | Appropriate Use of Healthcare |
| Patient-focused Episode of Care | |
| Risk Adjusted Total Cost of Care |
Table 1: Meaningful Measures from pp 6-7 of the FY 2019 Hospice Payment and Quality Reporting proposed rule
CMS noted their continued research into accounting for social risk factors in the Hospice QRP. They are planning to work with key stakeholders on identifying policy solutions that achieve the goal of attaining health equity for all beneficiaries and minimizing unintended consequences.
Perhaps CMS is taking a step back from rushing too quickly in creating the HEART tool. Designing an assessment that is meaningful and provides true measurement value to the consumer will take some time. Who says CMS doesn’t have a heart!
Did you know that 1,600+ hospices are using SHP's real-time data and benchmarking tools to improve quality? If you are not currently partnering with SHP, join us next week for a free webinar on May 9th. We will give an overview of our SHP for Hospice product and share how it helps hospices automate quality data tracking, support QAPI requirements, and manage CAHPS® Hospice surveys while improving scores.

