HHVBP – Managing under the new 2025 measure set
As of March 31st, Home Health Agencies (HHAs) will have three complete months of quality episodes under the new Performance Year (PY) 2025 measure set of the Expanded Home Health Value-based Purchasing (HHVBP) program. How is your HHA performing? It is not as easy as looking at your past HHVBP performances as there are some significant changes with PY 2025.
CMS not only reduced the number of measures from 12 to 10 (deleted 5, added in 3), but many of the measure weightings were also adjusted and the baseline year was changed from CY 2022 to CY 2023 reflecting more current outcome data. CMS did keep the ratio of measure weights across the OASIS/Claims/HHCAHPS categories the same at 35%/35%/30% respectively.
The new CY 2023 baseline year does have the effect of “raising the bar” on when HHAs would generate achievement and improvement points for each measure. For instance, in both PY 2023 & PY 2024 the median score to start to earn achievement points for Improvement in Management of Oral Meds (Oral Meds) was 80.99% (larger-volume cohort). In PY 2025, HHAs will need a score of 85.18% to earn any achievement points (see chart).
| Performance Year | Baseline Year | Achievement Threshold | Benchmark | Range | Average Care Points | Average Weighted Points |
|---|---|---|---|---|---|---|
| PY 23,24 | CY 2022 | 80.99 | 97.90 | 16.91 | 4.70 | 3.10 |
| PY 25 | CY 2023 | 85.18 | 98.75 | 13.57 | 3.31 | 3.30 |
| Percent Change | 5.2% | 0.9% | -19.8% | -29.6% | 6.5% |
In one example, a score of 85.00 would have earned 2.37 achievement points in the first two years of HHVBP, but no points in the third year. Using SHP’s national database, the Average Care Points for our clients (the higher of achievement or improvement points) using outcome scores from CY 2024 would decrease 1.39 points or 29.6% with the higher threshold. The only saving grace is the measure weight for Oral Meds did increase from 5.83% to 9.00% which ends up increasing the Average Weighted Points by 0.20 or 6.5%.
It should be noted that the new baseline year raises the bar for all agencies. For the seven of ten measures that didn’t change, the new thresholds and benchmarks will likely decrease the corresponding Care Points earned, as we see in the Oral Meds example, but the percentile rank for an HHA would likely not change since the impact affects all agencies alike. What about the new measures? Since all HHAs will have the same baseline year, the points earned will likely begin to increase as HHAs implement new quality improvement initiatives to get a jump on increasing both their improvement and achievement points.
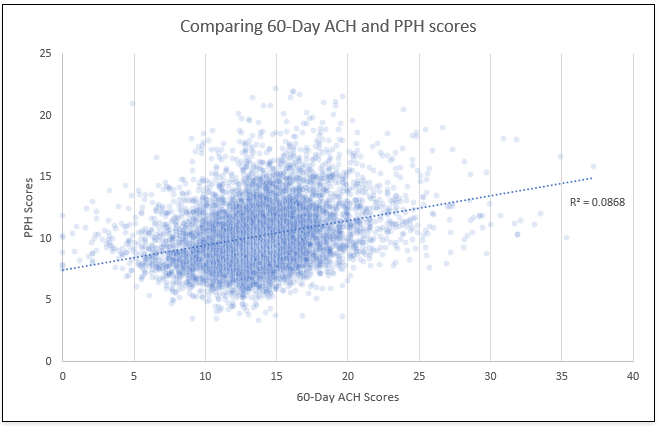
What is interesting about the new Potentially Preventable Hospitalization (PPH) claims-based measure is the impact of scores when compared to the now retired 60-day Acute Care Hospitalization (ACH) measure. Your agency may have good 60-day ACH scores, but that doesn’t mean you will be as successful with PPH. Using data from Care Compare and the CMS PY 2023 APRs, the correlation of agency scores shows a very small relationship (R squared = .087) between the two measures. The graphic below plots the points between each HHAs outcome values for the two measures.
To help prepare for the new measure set, CMS did share some helpful insights in the January 2025 Interim Payment Report (IPR). The “CY 2025 Baseline” tab shows each HHAs baseline score for 12 months of quality episodes ending in December 2023. For each measure, this value is the Agency Improvement Threshold, where higher scores in PY 2025 can earn improvement points.
It is also helpful that CMS shared the HHAs percentile ranking tier for your agency as well as the scores attributed at the 25th/50th/75th and 99th percentiles. HHAs can begin to set goals using these numbers. CMS does note these scores are listed as “Preliminary” and may change when finalized. Improving both measure outcome scores and percentile ranks is where a HHA will be successful. You want your scores to improve faster than HHAs in your cohort in order to achieve higher Total Performance Scores (TPS) scores and payment adjustments.
With the release of the SHP VBP Preview 2025+ report last year, HHAs can track in real-time how they are performing under the new measure set and not have to wait for the quarterly IPRs to catch up. Clients can track both their individual measure scores as well as percentile ranks for each measure and projected TPS scores using the SHP National database. Trending these scores across a rolling 12-months is a great way to track how your HHA is performing against the goals you set. Use this report to identify and drill into the measures needing improvement to help your HHA to be successful as you manage under the new PY 2025 measures set.
Get Ahead with SHP – Request Your Demo Today
Take the guesswork out of navigating the new 2025 HHVBP measure set with SHP’s advanced tools and real-time insights. Our VBP Preview 2025+ report empowers Home Health Agencies to track performance, identify improvement opportunities, and stay ahead of the curve. Request a demo today and discover how SHP can help your agency adapt, improve outcomes, and achieve success under the updated program. Reach out now—we’re here to help you excel!

