The Home Health Groupings Model (HHGM), which is the most significant change to the home health prospective payment reimbursement model since its inception, was finally released on Thursday, July 28th as part of the Home Health Payment Proposed Rule for CY 2018, although it is not scheduled to be implemented until CY 2019. Implementation could have started as early as January 1, 2018, but the National Association of Home and Hospice Care (NAHC) let the Centers for Medicare and Medicaid (CMS) officials know that rolling out the rule earlier than CY 2019 would severely disrupt its member organizations.
In a reversal of the original design posted by CMS in January 2017, the proposed HHGM is not budget neutral. As a result, reimbursements will be reduced by close to $1 billion per year, a significantly negative effect on the home health industry. NAHC argues, however, that CMS only has the authority to make budget neutral reimbursement changes. NAHC will make the argument that only Congress has the authority to make non-budget neutral changes through the legislative process.
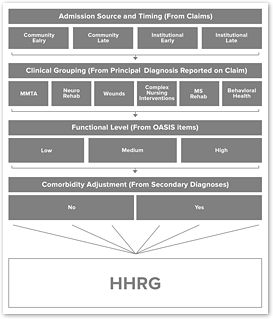
CMS, along with the Medicare Payment Advisory Commission (MedPAC), has long described the need for a new payment model that shifts from paying for volume to paying for value by eliminating therapy visits as a factor in payment determinations. CMS also wants to ensure that more complicated clinical cases are sufficiently compensated for their higher acuity. Accordingly, CMS will now use primary diagnosis to identify 6 clinical groupings for patient assignment.
Some of the other HHGM provisions include changes to the case mix scoring. The OASIS items used in the calculation of the functional score will include two new items: M1800 (Grooming), and M1033 (Risk for Hospitalization), in addition to the 6 that are used today.
Referral source, looking back 14 days from the start of care, will identify whether community or institution will be used in the model. Early and late will be determined by new 30-day billing periods with only the first 30-day period being defined as early. Finally, comorbidities will be added as another factor determining the patient’s clinical group assignment.
 Click to Enlarge
Click to Enlarge
Figure 1: Structure of the Proposed HHGM
Figure 1 shows the graph CMS published in the rule showing the groupings used in the new 144 HHRGs.
4 Admission Source and Timing categories
(x) 6 Clinical Groupings
(x) 3 Functional levels (x) 2 Comorbidity Adjustments
= 144 groups
CMS has also asked for comments on whether or not the Request for Anticipated Payment (RAP) should be eliminated. Let me guess your answer—no! Although not proposed in the first year, CMS clearly wants to phase out RAPs, and wants readers to comment on how to do this. CMS also discussed in the rule its rational for moving from a 60-day billing cycle to 30-day billing periods based on the frequency of visits over a typical 60-day episode model. CMS noted that approximately 25% of the time, episodes ended within 30 days.
The changes outlined in the proposed HHGM represent the most significant change to home health reimbursement since the implementation of the Home Health Prospective Payment System (HHPPS) in October 1999. To soften the blow, CMS includes the possibility of a partial budget-neutral adjustment, which could reduce the proposed reimbursement effect on organizations by nearly half in the first year. This would help in the short-term, but in reality only delays the full implementation by one year.
Now is the time to write your comments to CMS on the HHGM proposal. CMS will accept your comments until September 25th. Make sure your voice is heard by CMS and work closely with your national and state trade organizations that support your advocacy on HHGM.

