Are Physicians Contributing to Your Hospital Re-admissions?
Soon, no one in the healthcare continuum will be immune from quality measures, not even physicians. In late February, CMS announced that, for the first time, quality measures have been added to Physician Compare for group practices and ACOs. The new quality measures added to Physician Compare include:
- controlling blood-sugar levels in patients with diabetes;
- controlling blood pressure in patients with diabetes;
- prescribing aspirin to patients with diabetes and heart disease;
- patients with diabetes who do not use tobacco;
- and, prescribing medicine to improve the pumping action of the heart in patients who have both heart disease and certain other conditions.
But missing from these measurements is accountability for re-admissions!
Physicians play a big role in making the decisions that could ultimately lead to a re-admission, which in turn comes back to penalize home health agency performance scores – not a good situation when referral sources are looking to partner with agencies that demonstrate low hospitalization rates.
Just because CMS isn’t holding physicians accountable for this metric (yet!), doesn’t mean you can’t begin to measure and manage it yourself. You have a lot riding on those hospitalization and re-admission scores.
So, what tools are at your disposal?
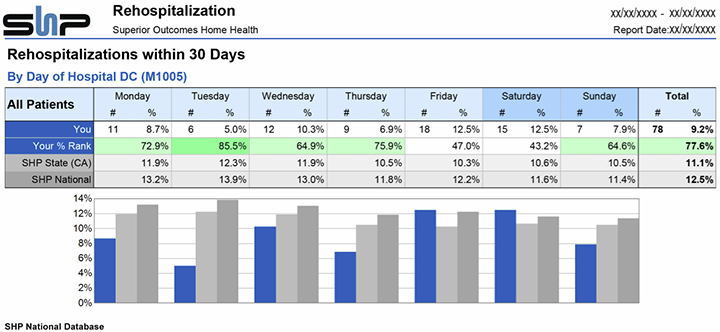
I suggest you look in three places to begin to determine if certain physicians or group practices are associated with more hospitalizations: 1) the SHP 30-day Readmission Report; 2) the SHP Hospitalization Report; and the 3) The SHP Physician Scorecard (this is a topic I’ll address in further detail in the March 12th Webinar, “Winning with ACOs and Hospitals”. If you’re not an SHP client, this is information I still suggest you obtain.
Start by running the Physician Overview report portion of the Physician Scorecard, and look for physicians with poor scores compared to the benchmark (which is highlighted in red). From there, drill down to the full Scorecard for more detail on the physicians of interest. Next, pull up the two hospitalization reports mentioned in the paragraph above. You’ll gain a lot of insight from the 30-day Readmission Report, and you can also evaluate referral source behavior to see if you might be receiving a higher than normal percentage of admissions on the weekend. If you’re noticing a lot of Friday and Saturday discharges, and your agency is not well-equipped to handle those, find out where they’re originating. Those patients may be at higher risk for readmission if they were discharged quickly with no follow-up scheduled for more than 72 hours.
Integrating measurement and data into your daily processes and holding individuals accountable is important, and physicians are no exception. Why not find one or two of your physicians who “get it” and make them champions of this change?