Recognizing the Importance of Oral Meds

As we draw closer to 2025, have you considered the huge impact Improvement in Management of Oral Medications (Oral Meds) will have in the upcoming year? Oral Meds play an integral part in all Home Health Quality Programs (HHQRP). Let’s break down each one and discuss best practices to ensure accuracy.
Star Ratings
There are seven measures used to calculate an overall star rating, and Oral Meds is one of them. We analyzed SHP’s 5-star agencies and their average overall Oral Meds scores came in at 96, while our 4.5 star agencies came in at 92, which provides you a comparative reference for how your agency is performing.
Home Health Value Based Purchasing (HHVBP)
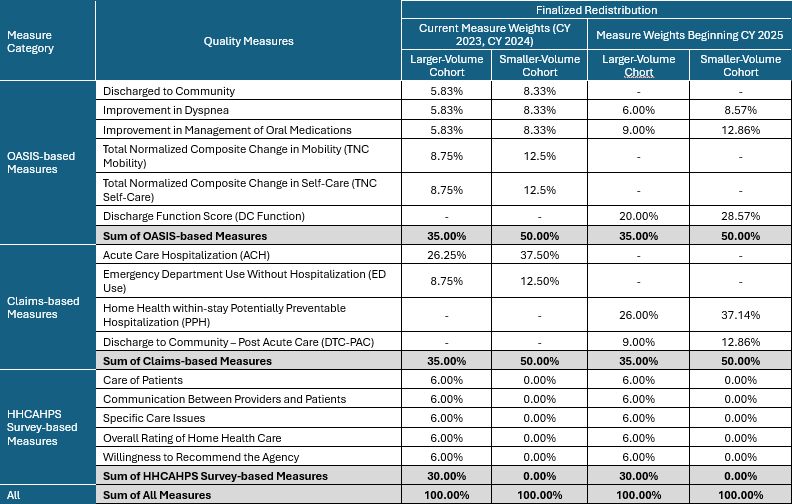
Starting in CY2025 the measure weights are increasing for Oral Meds. Under the previous program methodology, Oral Meds are weighted at 5.8 % for the larger-volume cohort and 8.3 % for the smaller-volume cohort. In 2025 this increases to 9.0% and 12.8% respectively. That’s a significant increase!
Furthermore, HHVBP has other measures that are impacted by Oral Meds. In CY2025 HHVBP now includes the new Discharge Function Score (DFS) measure. While medication management scoring isn’t included in the set of 10 items used in DFS Expected Score calculations, they are a covariate in the risk adjustments used to determine an expected score.
We also have the new Potentially Preventable Hospitalization (PPH) measure in HHVBP which is weighted 26.0% for the larger-volume cohort and 37.1 % for the smaller-volume cohort. Medication management can play a huge role in hospitalizations. The newly added Discharge to Community claims-based measure may be impacted by patients’ abilities to effectively manage their medications after discharge from home health services. This measure is weighted as 9% for the larger-volume cohort and 12.9% for the smaller-volume cohort.
Finally, the HHCAHPS portion of HHVBP, include Oral Meds related questions via the Specific Care composite that we discuss next.
HHCAHPS
Composite measures are included in the Expanded HHVBP, Care Compare and Star Ratings programs. The questions that make up the Specific Care Issues composite, assesses if someone talked to the patient about medications, allowed them to see medications, and explained the purpose and side effects of the medications. In HHVBP, the HHCAHPS measure category total is weighted as 30.0% for the larger-volume cohort.
Care Compare
Includes all the HHCAHPS questions from above, plus “How patients got better at taking their drugs correctly by mouth”, which is driven by the OASIS-based Oral Meds measure.
Best practices
So, what are some key steps to take at an agency level? Review OASIS guidance with your staff, which directs the clinician to assess a patients’ ability to take medications, rather than the actual performance of taking the medications. There are many factors we have to consider here. While OASIS guidance indicates we don’t need to assess a patients’ willingness or adherence, we do have to consider functional ability, where meds are stored, can the patient take the correct med at the correct time, can they open the bottles, etc.? Can they get to their meds? Can they read? Is their eye sight poor? Are they cognitively aware? There are many factors when determining the appropriate response.
Remind staff to make care plans focused on management of oral medications. Determine the root cause why a patient may not be compliant. Patient education is critical. In a lot of instances patients have no idea why they are taking a medication let alone potential side effects. Start the education as soon as possible and at a level the patient can comprehend easily. If you can educate them on their disease processes, how the medication can improve this, the effects of not adhering to their medications, and potential side effects, you may find increased compliance and new motivation for the patient to take them correctly.
Starting in CY2025 we see how important medication management is and the potential impacts it has for HHQRP. Focusing efforts in this area, will lead to improved patient outcomes, greater achievement levels in quality programs and healthier patients.
Don’t wait until 2025 to prioritize oral medication management! See how our tools and strategies can help your agency improve patient outcomes and quality program scores. Click here to request a demo and take the first step toward transforming your medication management processes today!

